Periodontitis, commonly known as advanced gum disease, is one of the most widespread chronic inflammatory conditions affecting adults worldwide. While many people associate gum disease strictly with oral complications bleeding gums, loose teeth, or bad breath modern research reveals that the impact of periodontitis goes far beyond the mouth.
In fact, the state of your gums may influence numerous aspects of your overall health, from cardiovascular function to metabolic balance and immune response. Understanding this connection is essential not only for dentists and medical professionals, but also for patients who may underestimate the systemic significance of oral hygiene.
Interestingly, in some discussions involving pharmaceutical distribution and healthcare supply chains, even topics like sourcing a mebendazole wholesaler come up alongside broader conversations about public health and access to care. This highlights how interconnected oral health, systemic health, and healthcare infrastructure truly are.
What Is Periodontitis?
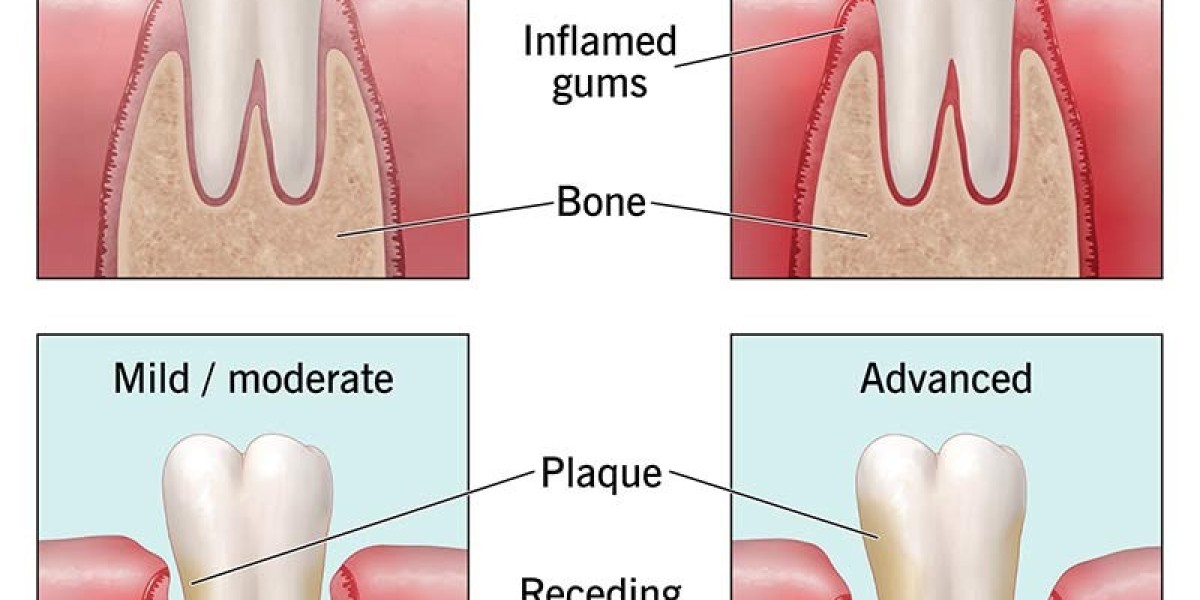
Periodontitis arises when plaqueb a sticky film of bacteria accumulates along the gumline. If plaque is not removed through regular brushing and flossing, it hardens into tartar, triggering inflammation known as gingivitis. When gingivitis is left untreated, it can progress into periodontitis, a more severe condition in which the gums pull away from the teeth, forming pockets that harbor harmful bacteria. Over time, this leads to bone loss, tooth mobility, and eventually tooth loss.
Yet the consequences are not limited to oral structures. The bacterial load and chronic inflammation associated with periodontitis have systemic effects, influencing organs and bodily processes far removed from the mouth.
Chronic Inflammation: The Core Link
One of the key mechanisms connecting periodontitis with systemic disease is chronic inflammation. Periodontal infections cause the immune system to launch an ongoing inflammatory response. Molecules such as cytokines, inflammatory mediators, and bacteria themselves can enter the bloodstream and travel throughout the body. When inflammation persists at a low but constant level, it becomes a major contributor to many chronic illnesses.
For instance, elevated inflammatory markers linked to gum disease like C-reactive protein (CRP) are also common indicators associated with heart disease, diabetes, and autoimmune disorders. This demonstrates that the inflammatory burden originating in the mouth may be an early warning sign or contributing factor in other health problems.
Periodontitis and Cardiovascular Disease
The relationship between gum disease and cardiovascular disease is one of the most studied systemic links. Researchers have found that people with periodontitis are at higher risk for:
Heart attacks
Stroke
Atherosclerosis (hardening of the arteries)
One theory is that periodontal bacteria enter the bloodstream and directly contribute to plaque formation within arterial walls. Another explanation is that chronic inflammation weakens blood vessels and promotes the buildup of fatty deposits. Regardless of the mechanism, the association is strong enough that cardiologists often encourage patients to maintain optimal oral hygiene as part of a comprehensive heart-health strategy.
Impact on Diabetes and Metabolic Health
Diabetes and periodontitis have a two-way relationship:
Poorly controlled diabetes increases susceptibility to gum infections.
Untreated gum disease makes it more difficult to control blood sugar levels.
Inflammation from periodontitis interferes with insulin signaling, contributing to insulin resistance. Meanwhile, high blood glucose levels create an environment where harmful oral bacteria thrive. This cycle can significantly worsen both conditions if not properly managed.
For individuals living with diabetes, regular dental checkups and early periodontal treatment can help support better glycemic control. Many endocrinologists now recognize oral care as a vital component of diabetes management.
Respiratory Complications
Another lesser-known connection involves the respiratory system. Bacteria from infected gums can be inhaled into the lungs, where they may contribute to conditions such as:
Pneumonia
Chronic obstructive pulmonary disease (COPD) flare-ups
Increased severity of respiratory infections
This is especially important for elderly patients and individuals with compromised immune systems. Maintaining a healthy mouth can significantly reduce the risk of microbial aspiration into the lungs.
Adverse Pregnancy Outcomes
Pregnant individuals should be particularly vigilant about gum health. Studies show that severe gum disease is associated with:
Preterm birth
Low birth weight
Preeclampsia
The inflammation and circulating bacteria linked to periodontitis may disrupt fetal development or trigger early labor. As part of prenatal care, obstetricians frequently recommend dental evaluations to help minimize these risks.
Autoimmune and Systemic Conditions
There is growing evidence that periodontitis may play a role in autoimmune and inflammatory disorders such as rheumatoid arthritis (RA). In some cases, specific oral bacteria are suspected of triggering autoimmune responses that attack joint tissues. Patients with RA often experience more severe gum disease, suggesting a shared inflammatory pathway between both conditions.
Researchers are also exploring potential relationships between periodontal disease and conditions like Alzheimer’s disease. Certain oral bacteria have been found in the brain tissue of Alzheimer's patients, although more studies are needed to establish a causal link.
The Role of Lifestyle and Access to Care
Oral health disparities contribute heavily to systemic health inequalities. Factors such as socioeconomic status, access to dental care, and education about proper oral hygiene all influence the prevalence and severity of periodontitis. Communities that lack reliable access to healthcare resources including medications, affordable dental services, or medical supply networks may face increased risk of both gum disease and chronic systemic illnesses.
This is one reason why public health discussions sometimes include topics like pharmaceutical supply chains and sourcing a mebendazole wholesaler or other essential medication distributors. Strengthening healthcare infrastructure across all levels from oral care to general medicine can significantly improve population-wide health outcomes.
Preventing and Managing Periodontitis
The good news is that periodontitis is largely preventable and, in many cases, treatable when caught early. Effective prevention strategies include:
Brushing at least twice daily
Flossing or using interdental cleaners
Scheduling regular dental checkups
Professional cleanings to remove tartar
Managing underlying conditions such as diabetes
Avoiding tobacco use
For advanced gum disease, treatments may involve deep cleaning (scaling and root planing), antimicrobial therapy, and in severe cases, periodontal surgery.
Conclusion
Periodontitis is far more than a dental concern it is a chronic inflammatory condition with profound implications for overall health. From cardiovascular disease to diabetes and respiratory complications, the evidence clearly shows that maintaining healthy gums is essential for maintaining a healthy body. As healthcare systems continue to emphasize preventive care, oral health must remain a priority. Whether discussing dental hygiene, chronic disease management, or even broader healthcare logistics like locating a mebendazole wholesaler, the message remains consistent: every component of the health system matters, and oral health is a foundational pillar of total well-being.